Post COVID Health Checkup near me in Greater Noida
Understanding Post COVID Health Checkup in Greater Noida
What is Post COVID Health Checkup in Greater Noida?
The infection of Coronavirus can have certain long term effects on health. It is suggested to go for some medical tests that helps in monitoring the overall health status of the patient who has recently recovered from the infection of Coronavirus. Post-COVID Health Checkup is a group of tests that include all relevant tests that help you keep a track of your health after you have suffered a COVID-19 infection. The tests screen the condition of heart, liver, kidney through the detection of specific markers. This package also detects antibodies developed post-COVID and the presence of any bacterial or fungal infection that can develop as a complication of COVID. The package helps you stay alert after the infection to determine whether or not you require medical attention.
What does Post COVID Health Checkup measure?
Contains 44 testsFollowing tests are a part of Post COVID Health Checkup:
Creatinine kinase (CK) isoenzyme electrophoresis is a test used to measure creatinine macro-enzymes in blood. These macro-enzymes are found in skeletal muscle, myocardium, and brain and their elevated levels may indicate a heart condition or other malignancies. Elevated levels of MB occur 4 to 6 hours after the onset of pain in myocardial infarction, peak at 18 to 24 hours, and persist up to 72 hours. BB isoenzyme increases in patients with a head injury and in some malignancies.
Kidney function test is a group of blood tests, which is used to determine how well the kidneys are working. KFT is performed either as a part of routine health checkups or to help diagnose any disease affecting the kidneys. It can also screen people at risk for the development of any kidney disease and even to monitor the treatment efficacy of kidney diseases.
Liver function test is used to assess the function of the liver and is done when any liver disease like viral hepatitis, alcoholic hepatitis, autoimmune hepatitis, and cirrhosis (scarring of the liver) is suspected. This test is also done for monitoring of any ongoing treatment or simply as a part of a routine checkup.
C-reactive protein quantitative test measures the level of C-Reactive Protein (CRP) in the blood. This protein is made in your liver in response to inflammation. Normally, you have low levels of CRP present in your blood. High levels can be indicative of serious infection or other disorders that include:
-Bacterial infections, like sepsis(sometimes a life-threatening condition)
-Fungal infection
-Inflammatory bowel disease
-An autoimmune disorder like rheumatoid arthritis or lupus
-A bone infection called osteomyelitis
Thyroid profile total is a group of tests that are done together to detect or diagnose thyroid diseases. It measures the levels of the following three hormones in the blood: Thyroid Stimulating Hormone (TSH), Thyroxine (T4) - Total and Triiodothyronine (T3) - Total. It is done to diagnose any suspected thyroid disease (Hypothyroidism or Hyperthyroidism). It also monitors treatment in patients with thyroid diseases.
Complete blood count (CBC) is a group of tests that provides information about your blood group and blood cells like Red Blood Cells (RBC), White Blood Cells (WBC), and platelets. It is routinely performed to provide an overview of a patient's general health status. it is also helpful in detecting a variety of disorders including infections, anemia, diseases of the immune system, and blood cancers and is done to monitor an existing blood disorder and its treatment such as chemotherapy or radiotherapy. NLR (Neutrophil to Lymphocyte Ratio) is a biomarker that shows inflammation in the body.
Covid IgG antibody test is a quantitative test for the detection of SARS-CoV-2 (COVID-19) IgG Antibodies after a person has been infected with COVID-19. A Positive test indicates past exposure to SARS-CoV-2. A negative test implies the absence of SARS-CoV-2 IgG antibodies hence immunity status cannot be established. IgG antibody usually becomes positive after 8 - 13 days of getting infected & is at the peak around 21 days after the infection.
Positive Antibody Testing: It shows exposure to SARS-CoV-2 (COVID-19) infection. This has importance in sero-surveillance/ epidemiology.
Negative Antibody test: It means that exposure to SARS-CoV-2 (COVID-19) infection is not established.

Lactate Dehyderogenase, Serum
Lactate dehydrogenase is an enzyme which plays an essential role in the production of energy from glucose. It is present in all the cells of the body, with the highest concentrations being in the cells of heart, lungs, muscles, liver, kidneys, and RBCs. Normally, only a small amount of the enzyme is found in the serum outside blood cells. However, in certain conditions of damage to the cells, lactate dehydrogenase is secreted out of the cells into the serum, where its concentration rises. Thus, the Serum Lactate Dehydrogenase Test is a nonspecific test that helps to determine the presence of conditions causing tissue damage somewhere in the body. Further tests are performed to identify the exact cause and location of these conditions.
The total lactate dehydrogenase in the body consists of five different forms of the enzymes (isoenzymes) named LDH-1 to LDH-5. The isoenzymes are present in different concentrations in different organs of the body. For example, LDH-1 and LDH-2 are most abundant in the cells of the heart, while LDH-5 is most abundant in the liver. Although the total LDH levels indicate tissue damage somewhere in the body, testing for the different isoenzymes can help identify the location of such damage.
Lactate dehydrogenase is also secreted into other body fluids in case of damage to the body tissues. It is also produced by bacteria and can be thus used to help identify bacterial meningitis.
Know more about Lactate Dehyderogenase, Serum

C- Reactive Protein Quantitative
CRP Test measures the levels of CRP in blood to detect the presence of an inflammation or to monitor the treatment and progress of an inflammatory condition. C-reactive Protein or CRP is an acute phase reactant protein which is produced and secreted by the liver in response to an inflammation in the body, which may be caused by tissue injury, infection, or autoimmune diseases. CRP levels increase in patients with trauma, heart attack, autoimmune diseases, bacterial infections, sepsis, post surgery, cancer, etc. CRP levels are often increased before the onset of other symptoms of inflammation such as pain, fever, etc. CRP levels in blood fall as the inflammation subsides.
It is a non-specific test. It can neither diagnose a condition by itself nor can it determine the location of a particular inflammation or disease. Other tests along with physical examination are performed to diagnose a particular condition and determine the location.
A variant of the CRP test is the High Sensitivity C-reactive Protein Test (hs-CRP) which is more sensitive for CRP levels and can detect blood CRP levels at a lower concentration than the standard CRP Test. The hs-CRP Test is performed usually to determine the risk of development of cardiovascular diseases in otherwise healthy individuals.
Know more about C- Reactive Protein Quantitative

Liver Function Test
LFT measures the level of liver enzymes, proteins, and bilirubin in the blood.
The liver is a wedge-shaped organ located in the right upper part of the abdomen. The liver helps in the synthesis of certain proteins, produces bile (an alkaline compound which helps in the breakdown of fat), process the bilirubin (a yellowish substance produced from the breakdown of hemoglobin) and helps in removing ammonia and other toxins (harmful substances) from the body. It plays an important role in the metabolism of fats, protein, and carbohydrates. It stores glycogen, vitamins, and minerals as well as helps in the metabolism (breakdown) of certain drugs.
Many diseases affect the health of the liver like hepatitis A, hepatitis B, hepatitis C, alcoholic hepatitis, autoimmune hepatitis, cirrhosis, non-alcoholic fatty liver disease (NAFLD), bile duct obstruction, liver or bile duct cancer and many others. Liver function can also be affected by various risk factors like alcohol abuse, certain drugs, sedentary lifestyle, and obesity. Regular monitoring of liver function is essential for early detection of any liver abnormality.
LFT is a group of tests that measure the levels of Aspartate Aminotransferase (AST), Alanine Aminotransferase (ALT), Alkaline Phosphatase (ALP), Total protein, Bilirubin and Gamma Glutamyltransferase (GGT) in blood. Each component has its own significance and helps to understand a particular aspect of the liver function.
Alanine Aminotransferase (ALT)
Alanine Aminotransferase (ALT) is an enzyme and this test measures the level of this enzyme in the blood. ALT is also known as serum glutamic-pyruvic transaminase (SGPT) and is mainly found in the liver, but also in smaller amounts in the kidneys, heart, pancreas and muscles. This enzyme is released into the bloodstream in case of liver disease or damage leading to increased ALT blood levels, a specific indicator of liver injury. However, this test cannot determine the extent or severity of the liver damage.
Aspartate Aminotransferase (AST)
This test measures the level of the enzyme AST in your blood. It is also known as serum glutamic-oxaloacetic transaminase (SGOT). AST is found in the liver and is released in the blood in large amounts in case of any liver injury. AST levels are usually measured along with ALT as AST is not specific for liver (also found in the heart, skeletal muscle and other organs). Your doctor may also recommend an ALT/AST ratio to help in the diagnosis.
Alkaline phosphatase (ALP)
This test measures the blood levels of the enzyme ALP which is found in the liver (one of the main source), bile ducts, bones, intestine, pancreas and kidney. ALP helps to break down proteins in the body. Diseases that mainly harm or damage the cells of the liver and bile duct, leading to overproduction and release of this enzyme into the bloodstream. This causes increased blood ALP levels.
Total Serum Protein
This test measures the total amount of protein in the blood, which includes two major types of proteins: albumin and globulin. The test report mentions separate results for total protein, albumin, globulin and albumin/globulin ratio (A/G ratio).
The level of proteins in the blood indicates the biosynthetic capacity of the liver. Hepatocytes (liver cells) are unable to synthesize this protein in certain liver diseases leading to a fall in protein levels in the blood.
Albumin is synthesized only in the liver. It helps to transports minerals, enzymes, hormones, bilirubin and some medicines throughout your body. It prevents the fluid from leaking out of your blood vessels into the tissues.
Globulin is synthesized in the liver and by the cells of the immune system. It plays a key role in fighting infections and transports many enzymes, hormones, minerals and some medicines in the body.
Bilirubin
This test measures the amount of bilirubin in the blood. Bilirubin is a waste product formed by the breakdown of red blood cells and is processed by the liver.
Bilirubin blood test report includes separate values for direct (conjugated) bilirubin, indirect (unconjugated) bilirubin, and total bilirubin.
When heme is released from the hemoglobin, it is converted to bilirubin. This is called unconjugated (indirect) bilirubin which is carried to the liver by some proteins.
In the liver, bilirubin gets attached (conjugated) to modified sugars (glucuronic acid) and form conjugated (direct) bilirubin.
Both these forms can be measured or estimated by laboratory tests, and a total bilirubin result (includes both direct and indirect bilirubin) is also measured.
A damaged liver can’t properly process bilirubin, leading to abnormally high levels of bilirubin in the blood. Increased unconjugated bilirubin in the blood results due to its overproduction or improper uptake by the liver. Increased conjugated bilirubin results can be seen in diseases that reduce the rate of secretion of conjugated bilirubin into the bile or the flow of bile into the intestine resulting in a backward flow of conjugated bilirubin into the blood.
Gamma-glutamyltransferase (GGT)
This test measures the level of the enzyme GGT in your blood which is present in large amounts in the liver. It is a transport molecule and it helps the liver to metabolize many drugs and toxins. GGT is a very sensitive test for detecting any liver disease especially due to alcohol abuse and is also one of the first enzymes to rise in patients with bile duct obstruction like tumor or stones.
Know more about Liver Function Test
Albumin
Bilirubin Indirect
Bilirubin Direct
Gamma Glutamyl Transferase
Protein Total
Bilirubin Total
The Bilirubin Total measures the amount of bilirubin present in the blood of a person. Bilirubin is an orange-yellow waste pigment produced by the normal breakdown of heme. The heme is a component of hemoglobin and is found in red blood cells. The liver processes the bilirubin and eliminates it from the body.
The life span of red blood cells is about 120 days. The heme which is released from the hemoglobin is converted into bilirubin which is called unconjugated bilirubin. It is then carried to the liver by proteins, where it gets attached to sugars and becomes conjugated bilirubin. This conjugated bilirubin enters the bile from the liver and passes to the small intestine. Here, it gets broken down by the bacteria and further gets eliminated in the stool. These breakdown products of bilirubin are responsible for giving the characteristic brown color to the stool.
A healthy adult body produces approximately 250 - 350 mg of bilirubin daily. About 85% of bilirubin comes from damaged or degraded RBCs while the remaining amount comes from the bone marrow or liver.
Small amount of unconjugated bilirubin is released in the blood normally, but there is no virtual presence of conjugated bilirubin in the blood.
Both the forms of bilirubin can be measured or evaluated by the laboratory tests, and total bilirubin (sum of conjugated or unconjugated bilirubin) may be reported. In case there is an increase in levels of bilirubin, there will be yellowing of the skin and white of the eyes, giving the appearance of jaundice.
Alanine Transaminase
Alanine Transaminase test measures the levels of alanine transaminase in the blood. Alanine Transaminase is an enzyme which is found in liver and kidney cells. However, this enzyme, in less quantity, can be found in the muscles and the heart. Its function is to convert alanine (an amino acid found in proteins) to pyruvate (intermediate in cellular energy production).
Generally, these levels of alanine transaminase in the blood remain low in healthy individuals. However, if there is any damage to the liver, alanine transaminase is released in the blood. This process helps in early detection of any damage to the liver.
The function of the liver is to process the nutrients of the body. It also produces bile which helps in digesting fats along with the production of other important proteins such as blood clotting factors and albumin. The liver breaks the potentially toxic substances into harmless products which can be used or eliminated by the body.
This test is done with another liver enzyme, aspartate aminotransferase (AST) as a part of the liver panel. In case of damage to the liver, there is a sudden rise in levels of both enzymes. However, alanine transaminase is more specific for the liver. In some cases, it is possible that only one of them is increased. The AST/ALT ratio can be calculated to differentiate between various causes and severity of the liver injury. This can also help to distinguish whether the injury is from damage to the liver or heart or muscles.
Alkaline Phosphatase
The alkaline phosphatase, serum test measures the alkaline phosphatase levels in the blood. Alkaline phosphatase (ALP) is an enzyme which is found in various tissues throughout the body. The maximum concentrations of ALP are present in cells of bone and liver. Usually, raised levels of ALP are caused due to liver disease or bone disorders.
ALP is found in the liver on the cell edges that join to form bile ducts. The bile ducts are the tiny tubes which drain bile from the liver to the bowels. The bile juice formed is required by the small intestine to help digest fat in the diet.
ALP is produced by osteoblasts cells in the bone which are involved in bone formation. The various tissue types produce distinct forms of ALP which are known as isoenzymes.
The levels of ALP generally increase to a great extent if one or more bile ducts get blocked. The reason could be inflammation of the gallbladder which is known as cholecystitis or the presence of gallstones. The small amount of increase of ALP in the blood can be seen in liver cancer and cirrhosis. These high levels can also be observed if there is intake of medications toxic to the liver and hepatitis.
In conditions, where there is formation of excessive bones such as Paget’s disease one can also have increased levels of ALP. Along with that, higher blood ALP levels can be seen in children and adolescents, as they are in the growing stage and so are their bones.
Aspartate Aminotransferase
Aspartate aminotransferase (AST) is an enzyme which is found in most of the body cells but mainly in the heart and liver. It is also present in kidneys and muscles but in smaller amounts. Normally, the levels of AST are low, but the levels rise when there is an injury to cells of the liver or muscle.
The function of the liver is to process the nutrients of the body. It also produces bile which helps in digesting fats along with the production of other important proteins such as blood clotting factors and albumin. The liver breaks the potentially toxic substances into harmless products which can be used or eliminated by the body.
The rise in levels of AST can be due to conditions causing liver damage such as hepatitis, drugs which are toxic to liver, cirrhosis, or alcoholism. The AST test is not specific for the liver. Its levels may also rise in conditions which affect other parts of the body.
This test is done with alanine aminotransferase (ALT) test. Both the enzymes are found in the liver and their levels rise in case of liver damage. The ratio of AST/ALT helps in differentiating between the causes of liver damage in case of injury to heart or muscle.
Globulin, Serum
Albumin/Globulin Ratio, Serum
Covid Antibody IgG (Quantitative)

Creatine Kinase
The Creatine Kinase Test measures the levels of Creatine Kinase in the blood. Creatine Kinase (CK) is an enzyme which is found in the brain, heart, skeletal muscle, and other tissues. In case of muscle damage, increased amounts of CK are released into the blood.
In the blood, normally small amount of CK is present which comes from the skeletal muscles primarily. In case of any damage to the muscle or interference with the production of muscle, energy can lead to increased levels of CK. Also, these levels may rise if there is any change with the use of muscle energy. The examples of such conditions include strenuous exercise and myositis (inflammation of muscles).
Muscle diseases (myopathies) such as muscle dystrophy can also lead to an increase in the levels of CK. However, significantly high levels of CK are observed in Rhabdomyolysis which there is an extreme breakdown of skeletal muscle tissue.
Know more about Creatine Kinase

Thyroid Stimulating Hormone, Ultrasensitive
Thyroid Stimulating Hormone (TSH) test measures the amount of TSH in your blood which helps to find out if the thyroid gland is working normally or not. Low TSH levels indicate hyperthyroidism and high TSH levels indicate hypothyroidism.
In case of hyperthyroidism, the thyroid gland produces very high amounts of thyroid hormones (T3 and T4) and you may experience symptoms of weight loss, rapid heartbeat, tremors, sweating, anxiety, increased sensitivity towards heat, etc. In case of Hypothyroidism, there is a decrease in the production of thyroid hormones (T3 and T4) which may cause weight gain, fatigue, slow heart rate, increased sensitivity towards cold, depression, dry and thin hair, etc.
There is a feedback system in the body to maintain stable amounts of the thyroid hormones (T3 and T4) in the blood. TSH signals the thyroid gland to make and release the thyroid hormones (T3 & T4) into the blood when the level of thyroid hormones is low and can also signal the thyroid gland to lower the production of thyroid hormones when the level of thyroid hormones is very high. So, when the thyroid hormone (T3 and T4) levels decrease, the pituitary gland is stimulated to release TSH and this high TSH level, in turn, stimulates thyroid gland to release more thyroid hormone (T3 & T4) from the thyroid gland and the vice-versa happens when the thyroid hormone levels are very high.
Know more about Thyroid Stimulating Hormone, Ultrasensitive

Kidney Function Test with Electrolytes
This is a test panel done to evaluate the kidney functions. It contains a group of tests integrated to collectively analyze any malfunction related to the kidney.
The kidneys are a pair of bean-shaped organs located on either side of the spinal column in the abdomen towards the back. The kidneys perform a number of important functions. The most important of these is that they filter the blood and separate the waste products generated out of regular metabolic activities of the body, primarily urea. Following the separation, the kidneys excrete the waste products out of the body through urine. They help in maintaining the normal pH level and water balance of the body. The kidneys also play essential roles in the synthesis of Vitamin D and Red Blood Cells (RBCs).
The Kidney Function Test includes the following tests to monitor kidney function:
· Blood Urea Nitrogen (BUN)/ Urea:
Blood Urea Nitrogen is a test to measure the amount of urea nitrogen present in the blood. Urea is a nitrogenous by-product formed by the metabolism of protein, and its level in blood serves as an indication of the amount of nitrogen present in blood as urea. In simpler terms, BUN is the measure of the amount of nitrogen present in blood in the form of urea. High BUN levels in the blood can be caused as a result of kidney diseases, dehydration and obstruction in the urinary tract due to kidney stones, prostate gland enlargement, etc.
Urea test measures the level of urea in the blood. Urea is a final waste product formed from the breakdown of proteins. Urea is filtered out of the blood by the kidneys to excrete excess nitrogen present in the blood through urine. Excess of urea in blood is called uremia and can be caused by a number of conditions including kidney diseases.
· Uric Acid:
This test measures the level of uric acid in the blood. Uric acid is a waste product formed from the breakdown of purines, which are essential building blocks of DNA. It is also produced by the metabolism of proteinaceous food, especially red meat. Uric acid is excreted from the body by the kidneys through urine and a small portion through stool. Although indirectly but uric acid test helps in estimating the proper functioning of the kidneys, .
The presence of excess amounts of uric acid in the blood is called hyperuricemia. This accumulation of uric acid crystals in the synovial fluid between joints lead to the formation of gouts. Hyperuricemia also causes the formation of hard lumps of uric acid crystals called tophi under the skin and at the top of the ears. Uric acid crystals can also accumulate in the kidneys and cause kidney stones.
· Creatinine:
This test measures the level of Creatinine in blood. Creatinine is a waste product formed from the normal breakdown of muscles in the body. Creatinine is almost completely excreted by the kidneys, so their levels in the blood serve as an indication of improper kidney function.
The levels of creatinine in the blood can rise due to decreased elimination from the kidneys as well as due to increased creatinine production by muscular breakdown, eating cooked meat, protein supplements, etc.
· BUN/Creatinine Ratio:
BUN/Creatinine Ratio compares the levels of nitrogen as urea in the blood to the levels of creatinine in the blood. This ratio serves as a more accurate representation of kidney function. An increase in the ratio can be seen in case of dehydration while creatinine levels remain the same. Low BUN to creatinine ratio can be caused due to a low protein diet, liver cirrhosis, rhabdomyolysis (muscle disease), syndrome of inappropriate antidiuretic hormone secretion (SIADH) as well as during pregnancy.
Electrolytes: The serum electrolyte test measures the following electrolytes:
Sodium (Na+)
Potassium (K+)
Chloride (Cl-)
Electrolytes play an important role in a number of body functions like metabolism, neuromuscular functioning, maintaining hydration, and pH (acid-base balance). Electrolytes also help in the entry of nutrients into the cells and removal of waste products from the cells. Electrolytes carry an electrical charge which can be either negative or positive and exist as dissolved salts in blood and body tissues. The Serum Electrolyte test measures the following important electrolytes:
Sodium (Na+)
Sodium is an essential body electrolyte which, along with potassium, chloride, bicarbonate, etc.helps to maintain the normal fluid and pH balance of the body. It is also vital for cellular metabolism, and in the activity of nerves and muscles and transmission of impulses between them. Sodium is present in all the body fluids. The highest concentration of sodium is found in blood and extracellular fluid.
Sodium is supplied to the body principally through dietary salt (sodium chloride or NaCl), and a small portion of sodium is absorbed through other food items. The required portion is absorbed by the body and the remaining is excreted by the kidneys through urine. The body maintains a very narrow range of sodium concentration by three mechanisms:
· Secretion of hormones natriuretic peptides and aldosterone to control sodium elimination through urine
· Secretion of antidiuretic hormone (ADH), also called Vasopressin, to control the volume of water eliminated through urine
· Induction of thirst
Any disruption in the above-mentioned mechanisms gives rise to an imbalance in the concentration of sodium in the blood to produce Hyponatremia (low blood sodium concentration), or Hypernatremia (high blood sodium concentration). Both these conditions produce a number of symptoms and may even lead to death.
Potassium (K+)
Potassium is one of the essential body electrolytes along with sodium, chloride, bicarbonate, etc. As an electrolyte, potassium helps to regulate the amount of fluids present in the body and to maintain a correct pH balance. It performs a vital role in cellular metabolism and transport of nutrients and waste products in and out of cells. It is also essential in the transmission of nerve impulses to muscles and muscle activity.
Sufficient amount of potassium required by the body is absorbed from dietary sources, and the remaining unabsorbed potassium is excreted by the kidneys. The hormone called aldosterone maintains the body potassium level within a small normal range. Aldosterone acts on the nephrons present in the kidneys and activates a sodium-potassium pump which helps the body to reabsorb sodium and excrete potassium. This helps to maintain the potassium concentration in the blood within its normal range. Deviation of potassium concentration from its normal range gives rise to Hyperkalemia (high potassium level in blood), or Hypokalemia (low potassium level in blood). Both these conditions may produce a number of symptoms, and may even be fatal if not controlled.
Chloride (Cl-)
Chloride is an essential mineral which acts as an electrolyte similar to potassium, sodium, bicarbonate, etc. It helps to maintain the normal fluid and electrolyte balance in the body. It also acts as a buffer to help maintain the pH balance of the body. It also plays an essential role in metabolism by producing hydrochloric acid (HCl) in the stomach for digestion. The highest concentration of chloride is found in blood and extracellular fluid (fluid present outside the cells).
Most of the chloride is supplied to the body through dietary salt (sodium chloride or NaCl), and a small portion is absorbed through other food items. The required portion is absorbed by the body and the remaining is excreted by the kidneys through urine. The concentration of chloride in blood is maintained within a very narrow range by the body. Its increase or decrease is directly correlated with the sodium levels.
Know more about Kidney Function Test with Electrolytes
Creatinine
Creatinine is a waste product which is produced by the muscles due to the breakdown of a compound called Creatine. During the cycle of energy production which is required to contract muscles, creatine is produced. Kidneys remove creatinine from the body by filtering it from the blood and then releasing it into the urine. This test measures the amount of creatinine in the blood.
The body produces creatine and creatinine at a relatively same rate. Since kidneys filter most of the creatinine from the blood and release it into the urine, the blood levels can be used as an indicator to know how well the kidneys are functioning. The amount of creatinine produced depends upon the size of the person as well as their muscle mass. That is why levels of creatinine are higher in men as compared to women and children.
Potassium
The Potassium Test measures the concentration of potassium in the blood.
Potassium is one of the essential body electrolytes along with sodium, chloride, bicarbonate, etc. As an electrolyte, potassium helps to regulate the amount of fluids present in the body and to maintain a correct pH balance. It performs a vital role in cellular metabolism and transport of nutrients and waste products in and out of cells. It is also essential in the transmission of nerve impulses to muscles and muscle activity.
Sufficient amount of potassium required by the body is absorbed from dietary sources, and the remaining unabsorbed potassium is excreted by the kidneys. Body potassium is maintained within a small normal range principally by the hormone aldosterone. Aldosterone acts on the nephrons in the kidneys and activates a sodium-potassium pump which helps the body to reabsorb sodium and excrete potassium. This helps to maintain the potassium concentration in the blood within its normal range. Deviation of potassium concentration from its normal range gives rise to Hyperkalemia (high potassium level in blood), or Hypokalemia (low potassium level in blood). Both these conditions may produce a number of symptoms, and may even be fatal if not controlled.
Uric Acid
The Uric acid test measures the levels of uric acid in the blood. Uric acid is a nitrogenous compound produced by the metabolic breakdown of purine. Purines are nitrogenous bases in DNA forming parts of the structural framework of the cells. Breakdown of purines occurs when cells become old and die, forming uric acid. Uric acid is also formed from the metabolic breakdown of some types of food like red meat, seafood, beans, etc.
Most of the uric acid in the blood is filtered and eliminated by the kidneys and a small remaining amount in the stool. The concentration of uric acid in the blood can increase due to overproduction of uric acid or improper elimination of uric acid, and this condition is called Hyperuricemia. Hyperuricemia can also be caused due to cancer treatment by chemotherapy or radiotherapy. These treatment methods kill the cancer cells, which may leak the uric acid into the blood.
Excess uric acid can form crystals in the synovial fluid between the joints causing inflammation and pain. This condition is called gout and can severely damage the joints if left untreated. The Uric Acid Test can indicate the presence of gout, or risk of formation of gout. However, it is not a definitive test for gout. Confirmatory test for gout is performed by analysis of synovial fluid (joint fluid) for monosodium urate crystals. Chronic Hyperuricemia can cause the formation of tophi, which are hard lumpy deposits of uric acid crystals formed under the skin, in the joints, and at the top of the ears. Tophi cause severe damage to the joints and may compress nerves causing chronic pain and disfigurement. The excess uric acid may also deposit and crystallize in the kidneys causing kidney stones and acute renal failure.
Chloride
Chloride is an essential mineral which acts as an electrolyte along with potassium, sodium, bicarbonate, etc. It helps to maintain the normal fluid and electrolyte balance of the body. It also acts as a buffer to help maintain the pH balance of the body. It also plays essential roles in metabolism. Chloride is used by the stomach to produce hydrochloric acid (HCl) for digestion. Chloride is present in all body fluids and is found in highest concentration in the blood and extracellular fluid (fluid present outside the cells).
Most of the chloride intake is through dietary salt (sodium chloride or NaCl), and a small portion through other food items. The body absorbs the required amount and the kidneys excrete the remaining through urine. The concentration of chloride in blood is maintained within a very narrow range by the body and usually increases or decreases in direct correlation with sodium levels.
Sodium
The Sodium test measures the concentration of sodium in the blood.
Sodium is an essential body electrolyte which, along with potassium, chloride, bicarbonate, etc., helps to maintain the normal fluid and pH balance in the body. It is also vital for cellular metabolism, and in the activity of nerves and muscles and transmission of impulses between them. Sodium is present in all body fluids and is found in highest concentration in the blood and extracellular fluid.
Sodium is supplied to the body principally through dietary salts (sodium chloride or NaCl), and a small portion of sodium is absorbed through other food items. The required portion is absorbed by the body and the remaining is excreted by the kidneys through urine. The body maintains a very narrow range of sodium concentration by three mechanisms:
· Secretion of hormones natriuretic peptides and aldosterone to control sodium elimination through urine
· Secretion of antidiuretic hormone (ADH), also called Vasopressin, to control the volume of water eliminated through urine
· Induction of thirst
Any disruption in the abovementioned mechanisms gives rise to an imbalance in the concentration of sodium in the blood to produce Hyponatremia (low blood sodium concentration), or Hypernatremia (high blood sodium concentration). Both these conditions produce a number of symptoms and may even lead to death.
Blood Urea Nitrogen (BUN)
The Blood Urea Nitrogen test measures the amount of urea nitrogen in the blood. Urea is a waste product which is formed in the liver. It is formed when protein is metabolized into amino acids. This leads to the production of ammonia which is further converted into urea which is a less toxic waste product.
Both ammonia and urea have nitrogen as their component. The liver releases urea into the blood which is then carried out to the kidneys. Here, it is filtered out of the blood and then released into the urine. Since this is a continuous process, a small and stable amount of urea nitrogen always remains in the blood.
In case of kidney or liver diseases, there is a change in the amount of urea present in the blood. If the liver produces urea in increased amounts or if there is any problem in the functioning of the kidneys, there can be difficulty in filtering out wastes of the blood which will lead to rising in urea concentrations in the blood. If due to liver damage or disease there is less production of urea, the concentration of BUN will fall.
The BUN test is done along with creatinine test to evaluate kidney function to diagnose kidney disease and to monitor patients undergoing treatment of kidney disease.

Complete Blood Count With NLR
Blood is composed of blood cells suspended in blood plasma (yellowish colored liquid). The blood cells include red blood cells (also called RBCs or erythrocytes), white blood cells (also called WBCs or leukocytes) and platelets (also called thrombocytes).
Red blood cells (RBCs) are the most abundant blood cells. RBCs contain hemoglobin which helps in the transportation of oxygen to the tissues. RBC count is the measurement of the number of RBCs in a given volume of blood.
Packed Cell Volume (PCV) or Hematocrit (Hct) is the measurement of the blood volume occupied by RBCs. It is expressed in percentage.
White blood cells (WBCs) are key components of the immune system and thus protect the body from various infections and cancers. Total Leucocyte count (TLC) is the measurement of the total number of leukocytes (WBCs) in a given volume of blood.
There are five types of WBCs:
Neutrophils
Basophils
Eosinophils
Lymphocytes
Monocytes
Neutrophil to lymphocyte ratio (NLR) is used as a marker of subclinical inflammation. It is calculated by dividing the number of neutrophils by number of lymphocytes, from peripheral blood sample.
Differential Leucocyte Count (DLC) determines the percentage of different types of WBCs.
Neutrophils, Basophils, and Eosinophils are called Granulocytes because of the presence of granules inside these cells.
Absolute count of different types of WBCs is the measurement of their absolute numbers in the given volume of blood.
Platelet count - Platelets (also called thrombocytes) are disc-shaped cell fragments without a nucleus that help in blood clotting. Platelet count is the measurement of the number of platelets in a given volume of blood.
Mean Platelet Volume (MPV) is a measurement of the average size of platelets.
PDW or platelet distribution width refers to the variation of platelet size distribution
Hemoglobin (Hb) - Hemoglobin (Hb) is a protein found in red blood cells (RBCs) that carries oxygen from the lungs to the body tissues, exchanges the oxygen for carbon dioxide, and then carries the carbon dioxide back to the lungs where it is exchanged for oxygen.
Mean Corpuscular Volume (MCV) is the average volume of a red blood cell.
Mean Corpuscular Hemoglobin (MCH) is the average amount of hemoglobin in the average red blood cell.
Mean Corpuscular Hemoglobin Concentration (MCHC) is the average concentration of hemoglobin in a given volume of red cells.
Red Cell Distribution Width Coefficient variation (RDW CV)is a measurement of the variability of red blood cell size and their mean size.
Know more about Complete Blood Count With NLR
Differential leucocyte Count
- Differential Neutrophil Count
- Differential Lymphocyte Count
- Differential Monocyte Count
- Differential Eosinophil Count
- Differential Basophil Count
Blood is made up of different types of cells which are suspended in a fluid called plasma. These include erythrocytes or red blood cells, leukocytes or white blood cells, and platelets. Blood cells are produced by the hematopoietic cells in bone marrow and are then released into circulation. RBCs carry oxygen to the tissues, platelets help in blood clotting at a site of injury, and leukocytes form an integral part of the immune system of the body.
WBCs are of five types, each having a different function and present in different numbers:
1. Neutrophils: Under normal conditions, the number of neutrophils present is higher than any other type of WBCs.. They provide protection against pathogens, mostly bacteria and sometimes fungi. Neutrophils engulf the pathogens completely and digest them (the process is called phagocytosis). They are usually associated with acute or short-term infections.
2. Eosinophils: Eosinophils are WBCs that are primarily responsible to fight parasitic infections. They are also involved in allergic reactions and regulation of the extent of immune response.
3. Basophils: Basophils are WBCs which are present in the lowest numbers in circulation. They are considered to play an important role in allergic response.
[Neutrophils, eosinophils, and basophils are together classified as granulocytes. Granulocytes are the WBCs which contain granules present in their cytoplasm. These granules secrete chemicals during immune response.]
4. Monocytes: Monocytes are WBCs which are also involved in protection against infectious pathogens by phagocytosis like neutrophils. However, monocytes are more commonly associated with chronic or long-term infections.
5. Lymphocytes: These are specialized WBCs which are responsible for recognizing and neutralizing foreign (non-self) cells and cancer cells in the body. Lymphocytes are of three types, all of which are differentiated from a common type of lymphocyte progenitor cell:
· T cells or T lymphocytes are produced in the bone marrow and mature in the thymus gland. They are responsible for differentiating between self and non-self cells of the body. T cells are also responsible for the initiation and extent of immune response, and targeted destruction of cancer cells and virus.
· B cells or B lymphocytes are control acquired immunity by producing antibodies against antigens found on foreign cells and pathogens like bacteria and viruses.
· Natural killer cells or NK cells destroy all foreign cells tagged by antibodies, cancer cells and virus-infected cells by phagocytosis.
Depending on various factors like age, gender, health condition, environmental factors, etc., varying amounts of different types of WBCs circulate in the blood. The bone marrow increases production of WBCs in response to an infection or inflammation anywhere in the body, which are then called to the site by a series of chemical signals, where they work to treat the condition. Depending on the condition, the count of one or more types of WBCs remains high in the blood. Once the condition subsides, WBC production by the bone marrow decreases and their count in circulation falls back to normal levels. Elevated amount of one or more types of leukocytes for a long time may be an indication of a chronic condition that is not resolving naturally and might need urgent attention.
Apart from an infection or inflammation, WBC count in blood can also be affected by other conditions like disorders of the immune system, autoimmune conditions, cancer, etc. One or more types of WBC count may be higher or lower than normal in these cases.
Differential Leukocyte Count Test serves as an indication of a condition affecting the body. Further tests are performed to confirm a particular condition and direct treatment.
This further contains
Red Blood Cell Count
Hemoglobin
The hemoglobin test measures the amount of hemoglobin in the blood.
Hemoglobin (Hb) is a protein found in red blood cells (RBCs) that carries oxygen from the lungs to the body tissues, and to exchange the oxygen for carbon dioxide. Hemoglobin then carries the carbon dioxide back to the lungs and where it is exchanged for oxygen. Iron is an essential part of hemoglobin. Most blood cells, including red blood cells, are produced regularly in your bone marrow (present within the cavities of many of large bones). To produce hemoglobin and red blood cells, your body needs iron, vitamin B12, folate and other nutrients from the foods you eat.
A decrease in hemoglobin concentration in blood results in anemia. Anemia is a blood disorder characterized by a decrease in the total amount of red blood cells (RBCs) or hemoglobin in the blood or a lowered ability of the blood to carry oxygen to body organs and tissues. Anemia is the most common blood disorder, affecting about a third of the global population and can cause symptoms like tiredness (fatigue), weakness, shortness of breath etc.
The hemoglobin test is usually performed as a part of complete blood count (CBC) test.
Platelet Count
The platelets will adhere to the injury site
The platelets will accumulate at the injury site
The platelets will release chemical compounds which stimulate gathering of other platelets
The platelet count measures the number of platelets present in the blood. Platelets are also known as thrombocytes which are tiny fragments of cells. These are formed from large cells which are found in the bone marrow known as megakaryocytes. After the platelets are formed, they are released into the blood circulation.
Whenever there is an injury to a tissue or blood vessel, bleeding starts. At this point, platelets help in stopping the bleeding in three ways:
With these steps, a loose platelet connection forms at the site of injury. This process is known as primary hemostasis. The activated platelets start to support the coagulation cascade which involves a series of steps that includes the sequential activation of clotting factors. This process is known as secondary hemostasis which results in the formation of fibrin strands that knit through the loose platelet connection to form a fibrin net. After that, the connection is compressed to form a stable clot so that it remains in place until the injury heals. Once the injury is healed, other factors come into play and break it down so that it gets removed.
In case the platelets are not sufficient in number or are not functioning properly, a stable clot might not form. These unstable clots can result in an increased risk of excessive bleeding.
Total Leucocyte Count
Blood is made up of different types of cells suspended in a fluid called plasma. These include erythrocytes or red blood cells, leukocytes or white blood cells, and platelets. Blood cells are produced by the hematopoietic cells in bone marrow and are then released into circulation. RBCs carry oxygen to the tissues, platelets help in blood clotting at a site of injury, and leukocytes form a part of the immune system of the body. WBCs are of five primary types: neutrophils, basophils, eosinophils, monocytes, and lymphocytes. Lymphocytes are further of three types: B-Lymphocytes, T-Lymphocytes, and natural killer (NK) cells. Neutrophils, basophils, eosinophils are collectively called granulocytes since they contain granules in cytoplasm.
Depending on various factors like age, gender, health condition, environmental factors, etc., varying amounts of different types of WBCs circulate in the blood. The bone marrow increases the production of WBCs in response to an infection or inflammation anywhere in the body. These WBCs are called to the site by a series of chemical signals, where they work to treat the condition. During this time, the total leukocyte count remains high in blood. Once the infection or inflammation subsides, WBC production by bone marrow decreases and WBC count in circulation falls back to normal levels. A continuously elevated WBC count may thus be an indication of a chronic condition that is not resolving naturally and might need urgent attention.
Apart from an infection or inflammation, WBC count in blood can also be affected by other conditions like disorders of the immune system, autoimmune conditions, cancer, etc. WBC count may be higher or lower than normal in these cases.
WBC count test serves as an indication of a condition affecting the body. Further tests are performed to confirm a particular condition and direct treatment.
Hematocrit
Human blood is made up of erythrocytes or red blood cells, leukocytes or white blood cells, and platelets suspended in a fluid called plasma. Each of the component of blood performs a specific function. The packed cell volume or hematocrit is a ratio of the volume occupied by the RBCs to the total volume occupied by all the blood components or whole blood.
The RBCs transport inhaled oxygen from the lungs to all the cells of the body, and also a small amount of carbon dioxide from the cells to the lungs to be exhaled. The majority of carbon dioxide is transported in solution in plasma as bicarbonate ions. They contain a protein called hemoglobin which binds to oxygen for transport.
RBCs are produced in the erythropoietic cells of the bone marrow in response to the hormone Erythropoietin secreted by the kidneys when oxygen saturation of blood is detected to be low (hypoxia). The average lifespan of RBCs in circulation is 120 days. Hence, the bone marrows continuously produce RBCs to maintain a steady concentration in blood. The Packed Cell Volume Test depends on the count as well as the average size of the RBCs (Mean Corpuscular Volume or MCV). Higher than normal amount of RBCs produced by the bone marrow can cause the hematocrit to increase, leading to increased blood density and slow blood flow. Lower than normal hematocrit can be caused by low production of RBCs, reduced lifespan of RBC in circulation, or excessive bleeding, leading to reduced amount of oxygen reaching the cells.
Mean Corpuscular Volume
Mean Corpuscular Hemoglobin
Mean Corpuscular Hemoglobin Concentration
Absolute Leucocyte Count
- Absolute Eosinophil Count
- Absolute Neutrophil Count
- Absolute Basophil Count
- Absolute Monocyte Count
This further contains
Mean Platelet Volume
PDW
Neutrophil Lymphocyte Ratio
RDW CV
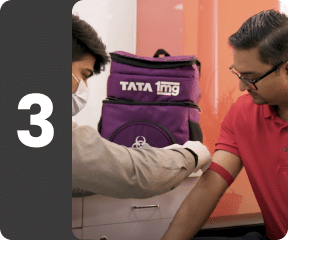
Book a Post COVID Health Checkup test at home near me


Other tests









